Department of Prosthodontics Institute of DY Patil University School
of Dentistry, Nerul, Navi Mumbai, Maharashtra, India.
Corresponding author email: drshresthkapoor24@gmail.com
Article Publishing History
Received: 20/06/2025
Accepted After Revision: 08/08/2025
Malpositioned dental implants in the anterior esthetic zone pose significant restorative and esthetic challenges. Conventional management often involves implant removal and re-placement with grafting, which can be invasive, time-consuming, and costly. This case report presents the prosthetic rehabilitation of a 26-year-old male with a malpositioned maxillary anterior implant managed using a digitally designed custom abutment. A digital impression was obtained and the abutment was designed using CAD software, followed by 3D printing of a resin prototype for trial verification. The definitive abutment was cast in cobalt-chromium alloy and restored with a porcelain-fused-to-metal crown incorporating gingival ceramic to compensate for soft tissue deficiencies. Esthetics were further enhanced with composite veneers on adjacent teeth. The prosthetic solution successfully corrected implant angulation, established a proper emergence profile, and provided natural esthetics and functional stability. This case highlights the clinical value of digital technologies and custom abutments in contemporary implant dentistry.
Custom abutment; malpositioned implant; CAD/CAM; digital dentistry; Anterior esthetics.
Singh R, Mistry G. S, Tabassum R, Parab S. B, Chabria A, Kapoor S. Digital Custom Abutment for the Prosthetic Management of a Malpositioned Anterior Implant: A Case Report. International Journal of Biomedical Research Science (IJBRS). 2025;01(3).
Singh R, Mistry G. S, Tabassum R, Parab S. B, Chabria A, Kapoor S. Digital Custom Abutment for the Prosthetic Management of a Malpositioned Anterior Implant: A Case Report. International Journal of Biomedical Research Science (IJBRS). 2025;01(3).. International Journal of Biomedical Research Science (IJBRS). 2025;01(3). Available from: <a href=”https://shorturl.at/S6g3o“>https://shorturl.at/S6g3oL</a>
INTRODUCTION
Dental implant therapy has become a predictable treatment modality for replacing missing teeth, with success dependent not only on osseointegration but also on correct three-dimensional positioning of the implant fixture [1]. Proper implant placement is particularly critical in the anterior maxilla, where esthetic and functional demands are high [2]. Deviation from the ideal prosthetic axis in this region often results in restorative challenges, including compromised emergence profile, impaired soft tissue contours, and suboptimal esthetic integration with the adjacent dentition.
Malposition of implants may occur due to anatomical limitations, inadequate treatment planning, or intraoperative complications [3]. Traditional management of such cases has involved implant removal followed by bone grafting and re-implantation in the correct position [4]. Although effective, these procedures are invasive, technique sensitive, time consuming, and associated with increased morbidity and patient cost [4,5]. An alternative prosthetic solution is the use of custom abutments, which allow correction of implant angulation, support of peri-implant tissues, and creation of a natural emergence profile without the need for additional surgery [6].
Recent advances in digital dentistry, including intraoral scanning, computer-aided design/computer-aided manufacturing (CAD/CAM), and additive manufacturing, have further enhanced the precision and predictability of custom abutment fabrication [7]. These technologies provide clinicians with the ability to design abutments that meet individualized esthetic and functional requirements in challenging scenarios [8]. The present case report describes the prosthetic management of a malpositioned anterior maxillary implant using a digitally designed custom abutment, highlighting the clinical steps, material selection, and outcome.
Case Report
Patient Information: A 26-year-old male reported to the Department of Prosthodontics with a requirement of restoring a previously placed anterior maxillary implant. The patient was in good systemic health, with no significant medical history or contraindications to prosthodontic treatment. He expressed dissatisfaction with the esthetics of his smile and difficulty in obtaining a functional restoration due to the malpositioned implant.
Clinical Findings: Extraoral examination revealed a balanced facial profile with adequate lip support and no signs of temporomandibular dysfunction. Intraoral examination demonstrated a single implant fixture placed in the maxillary anterior region with a pronounced labial angulation. The implant platform was positioned approximately 3–4 mm labial to the ideal prosthetic position (Figure 1). Despite the angulation, peri-implant soft tissues were healthy, and adequate keratinized tissue was present. Radiographic evaluation using periapical imaging confirmed satisfactory osseointegration without evidence of pathology, while also highlighting the extent of labial inclination.
Figure 1: Pre-operative photograph A) Occlusal view and B) Frontal view;
C) Checking Implant angulation; D) Sculpting of soft tissues around implant

Diagnostic Assessment: Based on the clinical and radiographic findings, the case was diagnosed as a malpositioned anterior implant with labial angulation requiring prosthetic correction. Two options were considered: surgical removal with bone grafting and re-implantation, or a prosthetic approach using a custom angulated abutment. After discussing the risks and benefits of both, the patient consented to the prosthetic solution.
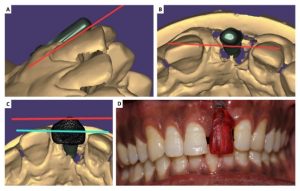
Therapeutic Intervention: The prosthetic rehabilitation began with digital impressions obtained using the open-tray technique with polyvinyl siloxane impression material. The impressions were scanned to generate a digital model, which was used in CAD software to design a custom abutment capable of correcting the angulation and establishing an appropriate emergence profile. A resin prototype of the abutment was fabricated through 3D printing and trial-fitted to verify adaptation, soft tissue response, and esthetics (Figure 2). After successful evaluation, the final abutment was cast in a cobalt-chromium alloy, finished, and polished for clinical use.
Figure 2: A), B), and C) 3-D designing of the prosthesis; D) Trial of the 3D-Printed resin prosthesis
Soft tissue sculpting was carefully performed during the trial and final placement phases to condition the peri-implant mucosa and optimize papillary form. The definitive prosthesis was fabricated as a porcelain-fused-to-metal crown incorporating gingival ceramic to compensate for soft tissue deficiency in the cervical region. The restoration was cemented with a resin-modified glass ionomer cement, ensuring proper retention and marginal seal. To further enhance esthetics and create harmony with the adjacent dentition, direct composite veneers were placed on teeth #11 and #22 using a nanohybrid composite system with enamel-bonding adhesive.
Follow-Up and Outcomes: The patient was reviewed at regular intervals to assess the health of peri-implant tissues, prosthesis integrity, and esthetic stability. The custom abutment corrected the unfavorable implant angulation and provided a natural emergence profile, while the PFM crown with gingival ceramic restored both esthetics and function (Figure 3). The adjacent composite veneers contributed to an improved smile line and overall harmony. The peri-implant tissues remained stable, with healthy mucosa and no signs of inflammation or bone loss. The patient expressed satisfaction with the functional and esthetic results.
Figure 3: A) Custom abutment and B) Cemented Final Prosthesis

DISCUSSION
The management of malpositioned implants, particularly in the anterior maxilla, remains one of the most demanding challenges in implant prosthodontics due to the high esthetic expectations and the complex anatomical constraints of the region [4,9]. In the present case, the use of a custom abutment fabricated through a digital workflow allowed the correction of the labial angulation of the implant and provided an emergence profile that harmonized with the adjacent dentition. This approach not only avoided the need for implant removal and grafting procedures, which are associated with increased morbidity and cost, but also preserved the osseointegration of the existing implant, thereby minimizing patient discomfort and treatment duration[10].
Custom abutments have been shown to provide distinct advantages over prefabricated stock abutments, especially when implant placement deviates from the ideal axis [8,11]. They facilitate precise correction of angulation, improved soft tissue support, and the development of natural gingival contours, which are critical to achieving esthetic success in the anterior zone [12]. The integration of CAD/CAM and 3D printing technologies further enhanced the predictability of the treatment by allowing virtual planning, prototyping, and clinical verification before final fabrication [13]. This digital workflow not only improved accuracy but also optimized communication between the clinician and the laboratory, leading to a more controlled and efficient process [13].
Material selection also played a significant role in the clinical success of the present case. The use of a cobalt-chromium alloy for the abutment provided adequate mechanical strength and biocompatibility, while the porcelain-fused-to-metal crown with gingival ceramic compensated for tissue deficiencies, ensuring seamless esthetics [14]. Additionally, the placement of composite veneers on adjacent teeth enhanced smile harmony, underscoring the value of a comprehensive esthetic approach [15].
The outcome of this case is consistent with existing literature that supports the use of custom abutments for malpositioned implants, with studies reporting high survival rates and long-term stability of peri-implant tissues when such prosthetic solutions are employed. While the cost and technical demands of custom abutments may be higher compared to stock abutments, the benefits in terms of esthetics, function, and patient satisfaction justify their use in challenging cases [13-15]. Moreover, as digital technologies continue to evolve, the process of designing and fabricating custom abutments is becoming increasingly streamlined and accessible, further reinforcing their clinical relevance [10,11].
The present case, therefore, highlights the importance of careful treatment planning, patient-centered decision making, and the integration of modern digital tools in overcoming the limitations imposed by implant malposition. By adopting a prosthetic rather than surgical approach, predictable esthetic and functional outcomes were achieved while minimizing invasiveness, underscoring the value of custom abutment therapy in contemporary implant dentistry.
CONCLUSION
The present case report demonstrates the successful rehabilitation of a malpositioned anterior implant using a digitally designed and custom-fabricated abutment, which corrected the implant angulation and restored a natural emergence profile. The prosthetic approach eliminated the need for invasive surgical intervention while achieving optimal esthetics, function, and patient satisfaction. Custom abutments, supported by digital technologies, represent a predictable and conservative solution for managing challenging implant positions in the esthetic zone.
REFERENCES
- Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology 2000. 2017 Feb;73(1):7-21.
- Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. International Journal of Oral & Maxillofacial Implants. 2004 Nov 2;19(7).
- Chen ST, Buser D, Dent M. Esthetic complications due to implant malpositions: etiology, prevention, and treatment. Dental implant complications: etiology, prevention, and treatment. 2015 Nov 16:209-32.
- Chen ST, Buser D, Sculean A, Belser UC. Complications and treatment errors in implant positioning in the aesthetic zone: diagnosis and possible solutions. Periodontology 2000. 2023 Jun;92(1):220-34.
- Alaqeely R, Albaiz A, Alenazi B, Alem M, Alotaibi Y, Alrowis R. Prevalence of Dental Implant Positioning Errors: A Radiographic Analysis. Journal of Clinical Medicine. 2025 May 6;14(9):3221.
- Pathak A, Dhamande MM, Sathe S, Bhoyar A, Gujjelwar S. Rehabilitation of malpositioned implant in the anterior region with customized abutment. Cureus. 2023 Dec 13;15(12).
- Gallo S, Pascadopoli M, Pellegrini M, Pulicari F, Manfredini M, Zampetti P, Spadari F, Maiorana C, Scribante A. CAD/CAM abutments versus stock abutments: An update review. Prosthesis. 2022 Aug 16;4(3):468-79.
- Târtea DA, Ionescu M, Manolea HO, Mercuț V, Obădan E, Amărăscu MO, Mărășescu PC, Dăguci L, Popescu SM. Comparative study of dental custom CAD-CAM implant abutments and dental implant stock abutments. Journal of Clinical Medicine. 2023 Mar 8;12(6):2128.
- Akmal O’g’li JE. COMPLICATIONS AND ERRORS IN IMPLANT PLACEMENT IN THE ESTHETIC ZONE: DIAGNOSIS AND POTENTIAL SOLUTIONS. Journal of Modern Educational Achievements. 2024 Oct 23;10(10):209-13.
- Lopo Barros JH, Oliveira MN, Cardoso IO, Oliveira GJ, Prado CJ, Neves FD. Computer-Aided Design/Computer-Aided Manufacturing of Customized Abutment for Rehabilitating a Malpositioned Implant Using Digital Flow: A Case Report. InHealthcare 2023 Sep 6 (Vol. 11, No. 18, p. 2472). MDPI.
- Barwacz CA, Swenson M, Couso‐Queiruga E, Comnick C, Xie XJ, Avila‐Ortiz G. Effect of CAD/CAM Abutment Morphology on the Outcomes of Implant Therapy: A Randomized Controlled Trial. Clinical oral implants research. 2025 Mar;36(3):374-85.
- Tramontana D. Custom Abutments for Dental Implants, Their Evolution and Uses: A Narrative Review. PQDT-Global. 2022.
- Bida C, Virvescu DI, Bosinceanu DN, Luchian I, Fratila D, Tunaru O, Bulancea B, Cretu OC, Surlari Z, Budala DG. Advances in dental prosthetics: The role of CAD/CAM technology in denture fabrication. Romanian Journal of Medical and Dental Education. 2024 Jan;13(1).
- Fratila A, Jimenez-Marcos C, Mirza-Rosca JC, Saceleanu A. Mechanical properties and biocompatibility of various cobalt chromium dental alloys. Materials Chemistry and Physics. 2023 Aug 1;304:127867.
- Coelho de Souza FH, Fagundes HH, Melecchi PV, Machado LS. Prefabricated composite veneers: na efficient alternative in smile aesthetic rehabilitation-a case report. Advances in Dentistry & Oral Health. United States. Vol. 18, no 2,(2025), 11 p.. 2025.



